Joslin Diabetes – Making Beta Cells
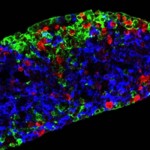
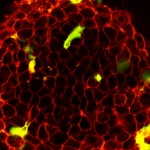
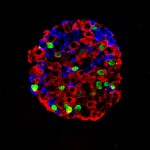
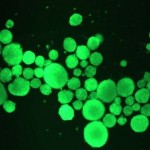
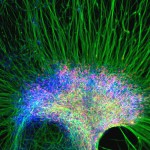
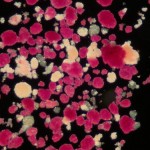
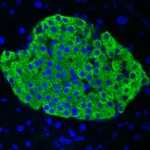
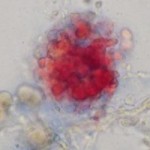
A new technique developed over the last decade can take skin cells, or any other cells of the body, and make them into something new. This process holds promise for the damaged pancreas of people with diabetes.